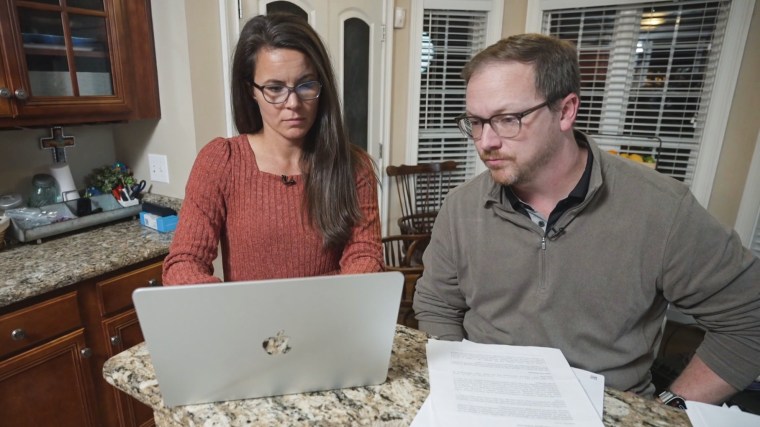
When insurance twice refused to cover a nearly $800,000-a-year drug that Paxton Pope’s doctor believed could dramatically reduce his frequent seizures, his family initially braced for a serious medical setback.
Then the Popes, of Davidson, North Carolina, learned about a little-known provision in the Affordable Care Act that allows asking an outside state-run panel to review the insurer’s decision — a move that led to the denial ultimately being overturned.
In the few months since then, access to the drug has already transformed the 13-year-old’s life, according to his mother, Maggie Pope. Paxton went from as many as 12 seizures an hour to about eight a day, she said, and he’s regaining skills he had started to lose, like holding conversations and telling them what he’s reading in school. For the first time, he’s able to play on his school’s flag football team.
“I was just over the moon,” Maggie Pope said. “I looked over at him, and he was just smiling. I said, ‘Paxton, did you know you were having less seizures?’ And he just kind of shook his head, ‘Yeah.’”

The denial was overturned by the North Carolina Department of Insurance, a state agency that oversees health insurers and helps patients challenge denied claims.
Every state has some form of insurance department or commission, although what programs they offer and the amount of resources they have can vary. Experts say that while most patients don’t know these agencies exist, they can guide individuals or families through an additional step beyond the insurer’s internal appeals process: an external review.
If you are dealing with bills that seem to be out of line or a denial of coverage, care or repairs, whether for health, home or auto, please email us at [email protected].
Under federal law, if a doctor says a treatment is medically necessary but an insurer still denies it, requesting an external review sends the case to an independent panel, which assigns it to a doctor to review the claim and issue a binding decision.
“They’re a well-kept secret,” said Michele Johnson, executive director of the Tennessee Justice Center, a law firm and nonprofit advocacy group that helps people dispute medical bills. “I think it’s definitely worth trying, and get doctors to help fight for you, because, of course, the doctor’s opinion is going to make a huge difference.”
‘My heart would break’
Millions of people in the U.S. have claims denied each year.
A 2023 survey from KFF, a nonpartisan health policy research group, found that 58% of insured adults said they’ve experienced a problem using their health insurance, including denied claims. That same year, nearly half of Americans got a medical bill that should’ve been covered, according to The Commonwealth Fund, another nonpartisan health policy research group.
Most people don’t realize they have options after a denial, and even less know a state office exists to help, said Art Caplan, the head of the medical ethics division at NYU Grossman School of Medicine in New York City. “They give up on the first scenario,” he said.
The Popes realized they could request an external review when they noticed a line at the bottom of the second denial letter they received for Paxton’s drug. It said they could take the case to the state insurance commission.
“They had pretty clear steps,” Maggie Pope said.
Paxton has a rare genetic condition caused by a mutation in a gene called SLC6A1. The mutation can result in childhood-onset epilepsy, developmental delays and movement disorders, according to the Children’s Hospital of Philadelphia.
Paxton’s doctor wanted him to take Ravicti, a drug that’s approved for urea cycle disorders. It’s not approved for Paxton’s condition, but early research suggests it may help reduce seizures linked to the SLC6A1 gene.
Paxton’s father, Greyson Pope, said they were afraid that without the medication, he would die from the seizures or “we would lose those things that made him himself, that we would be left with a shell of who he was.”
“Every time I saw a seizure, a little piece of my heart would break,” Maggie Pope said. “It’s debilitating to watch someone you love come in and out of cognition and reality. … There was definitely some anger every once in a while, where you just get frustrated that we couldn’t help him.”

Far from ideal
There was no guarantee that requesting an external review would lead to the Popes’ denial being overturned.
The state program that handles denied claims, called Smart NC, has overturned 153 cases out of the 282 it’s received this year through November — about 53% — according to Barry Smith, the deputy director of communications at the North Carolina Department of Insurance.
Other state insurance agencies have seen similar rates: Kansas has an overturn rate of 54% since 2018; California has overturned 51% of cases over the last 10 years; Colorado overturned 44% of cases last year; and South Carolina reversed 43% of cases in 2024. Other states saw lower rates: Washington state’s overturn rate was 25% in 2024, and West Virginia’s is 17% over the last five years.
North Carolina Insurance Commissioner Mike Causey said the agency manages thousands of cases each year. Beyond external reviews, the agency helps people with surprise medical bills, prior authorization issues and Medicare fraud.

“Our job is to enforce laws and to regulate insurance and to make sure that the companies are fair,” Causey said.
Still, Johnson, of the Tennessee Justice Center, said the process is far from ideal, noting that her frustration is aimed at the broader health care system, not the state office.
Most families dealing with serious medical issues can’t afford to wait weeks or months for an appeal — and navigating the paperwork can feel impossible when you’re caring for a sick child. “If you’re a regular person trying to navigate this process, it’s often really overwhelming and challenging,” she said.

Maggie Pope said the family had to do a pre-application to see if they were eligible for an external review, including providing paperwork on the two denied claims and medical tests on Paxton’s seizures.
Paxton’s doctor first submitted the prescription request to their insurance on April 17. By May 20, the family had been denied twice by their insurance. In June, Maggie Pope said she submitted the paperwork to the state agency for the external appeal. On Aug. 5, they got a letter that the denial had been overturned.
“I was thankful for this whole process,” Maggie Pope said. “It was really only a five-month window of time from the time we submitted the prescription to the time we got it.”
Greyson Pope said the family wants to raise awareness that resources like the North Carolina Department of Insurance exist.
“Just because you got one no or even two noes, it doesn’t have to be the end of the story,” he said.



